
Research shows that many Americans believe that everyone should have access to affordable health care coverage.
However, the method to achieve that goal remains a topic of national debate. ]There are many paths to achieving “universal coverage” both nationally and at the state level; the details of which are often overlooked or misunderstood.
The purpose of this brief is to examine the terminology and methodology underpinning this important conversation to support an informed dialogue grounded in fact.
How is universal coverage defined?
Universal coverage means that everyone has access to good quality health services without suffering financial hardship.1 Kaiser Permanente supports universal coverage and believes that everyone in America should have access to high-quality comprehensive health care coverage they can afford.
A solid majority of Americans (91%) have some form of coverage (figure 1).2 That leaves on average about 9% of Americans without coverage, but that’s nowhere near the full story: Many people move in and out of coverage, and the source of coverage (employer, government, or self) changes as well. Further, the sufficiency of coverage – whether it provides effective access to health care without causing financial hardship – varies greatly.
The Patient Protection and Affordable Care Act (ACA), with its goals of expanding both the number of people covered as well as improving the sufficiency of coverage, has improved access to and affordability of health coverage for Americans ( figure 2).3 However, the ACA alone has not achieved true “universal” health coverage.
How do single-payer models relate to universal coverage? 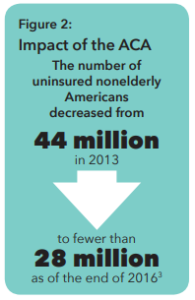
Single- and multi-payer models describe possible structures to finance the costs of a health care system. Single-payer refers to a single, centralized, publicly organized means to collect, pool, and distribute money to pay for the delivery of health care services for all members of a defined population.4
Although definitions and classifications may vary somewhat by analyst, most experts agree that there are five or six types of types of health care systems used around the world, and only two of them are true single-payer models. Countries have used both single- and multi-payer models to achieve the outcome of universal coverage, but no two countries’ systems are identical.
What’s the best path toward universal coverage?
Americans remain uncertain about the best path forward. A February 2017 Pew Research Center poll found that 54% of the public approved of the ACA,5 while a June 2017 poll found that 33% now favor a single payer approach.6 Of those who disapprove of the ACA, 25% want congressional leaders to focus their efforts on modifying the law rather than on getting rid of it (17%).
At Kaiser Permanente we believe we must unite around the goal of universal coverage and that the best way to achieve this goal is to continue building on the progress made over the past decade, with tens of millions of people gaining coverage in a system built on a strong partnership between the private and public sectors.