
Integrated Care Stories
Cutting cancer risk through targeted expansion of genetic testing
Kaiser Permanente achieves better outcomes through a combination of care coordination, comprehensive data collection and use, and aligned incentives that all promote affordable, high-quality care. This case study, part of our Integrated Care Stories series, highlights the benefits of Kaiser Permanente’s approach.
The challenge
In the United States, 1 in 400 women inherit mutations in BRCA1 or BRCA2, genes that repair damaged DNA.1 Harmful BRCA1 and BRCA2 gene mutations dramatically increase the risk of breast and ovarian cancer.
While 12% of women in the general population will develop breast cancer in their lifetimes, 72% of women with a harmful BRCA1 mutation will, as will 69% of women with a BRCA2 mutation. Similarly, only 1% of women in the general population will develop ovarian cancer, compared to lifetime risk as high as 44% for women with a BRCA1 mutation, and 17% for women with a BRCA2 mutation.2 In addition to the well-known risks of BRCA1 and BRCA2, there are at least 32 additional genes associated with breast and ovarian cancers, and some bring additional cancer risks.
Genetic testing can identify these mutations, and interventions can greatly reduce health risks. To realize these benefits, however, women need timely screening and support throughout the testing and treatment process.
The integrated care and coverage solution
Kaiser Permanente created a hereditary cancer program to address this challenge
Care teams identify and educate high-risk patients about their genetic risks and provide coordinated support.
These care teams include experts in genetics, breast care, gynecologic cancer, plastic surgery, and supportive services. They work with women who have a harmful genetic mutation to develop and implement tailored cancer prevention plans, which might include more frequent screenings, a preventive bilateral mastectomy to remove high-risk tissue, reconstructive surgery, surgery to remove the ovaries and fallopian tubes, or chemopreventive drugs. These decisions are complex and will vary depending on each woman’s personal goals and preferences, so members benefit from the support of this coordinated team of experts.
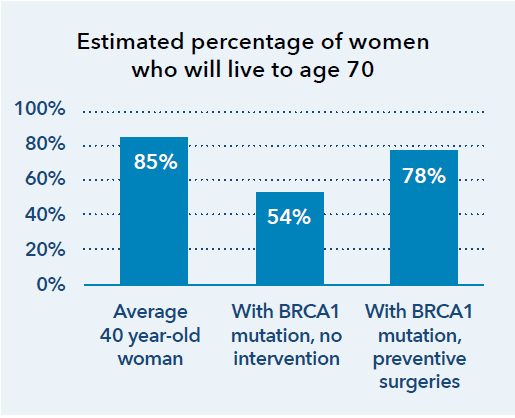
Interventions can have a dramatic impact, greatly improving life expectancy,3 while also reducing costs.4
How Kaiser Permanente’s integrated care and coverage model supported this innovation
High-quality care, with clinical decisions made by doctors and patients
Physicians work with their patients to develop personalized care plans, making decisions about medical care together. To inform those decisions, doctors use the best available evidence and create clinical practice guidelines. They champion quality improvement, ensuring that our care teams practice medicine based on the best, most up-to-date information, incorporating innovative approaches.
Bethan Powell, MD, an innovator working to address cancer risk since the first discovery of the BRCA gene mutations in the early 1990s, launched the first Hereditary Cancer Center at Kaiser Permanente San Francisco in 2008. She collaborated with physician colleagues to expand to a network of 6 Kaiser Permanente Hereditary Cancer Centers throughout Northern California.
Flexibility within a budget
The Kaiser Foundation Health Plan collects member premiums in advance and then pays delivery system partners for members’ care throughout the year. This creates the flexibility within and across the health plan, the hospitals, and the medical groups to deploy those resources to best meet our members’ needs. Instead of relying on revenues generated when patients are sick, we are incentivized to invest in longer-term infrastructure and population health investments that improve long-term outcomes and to provide timely, effective, and efficient care and service.
Kaiser Permanente Hereditary Cancer Centers improve patient health and save costs through preventive steps that reduce the need for avoidable, costly medical interventions later. When women who are at high risk intervene early, many will never develop these cancers and will never need chemotherapy or radiation treatments. Early treatment increases the odds that they will live long, healthy lives.
Integrated data for each member
Members can easily access their personal data through Kaiser Permanente’s comprehensive, interconnected data system. They can see detailed health information, connect with their care team, and access telehealth services through kp.org, our secure, web-based member portal.
Women with a harmful gene mutation must coordinate with health care professionals across specialties to understand their risks and options. At Kaiser Permanente, they can consult with multiple specialists, including a genetic counselor, a gynecologist, a gynecologic surgeon, a breast surgeon, and a plastic surgeon. Through Kaiser Permanente’s web-based member portal, our members can easily access information and coordinate with their care team.
Connected, coordinated care teams
Clinicians can easily coordinate with one another and seamlessly refer patients to other team members — primary care doctors, specialists, lab technicians, pharmacists, and other health care professionals.
The full Hereditary Cancer Program care team meets as a group to discuss the patient’s case and then meets with the patient to understand her goals and discuss treatment options. By working together, the patient and care team have the information they need for decision-making and can easily and effectively coordinate care.
Kaiser Permanente’s integrated care and coverage model differs from much of the United States health care system, which relies on disconnected clinical practices paid through fee-for-service. These disconnected approaches typically result in highly fragmented care, a focus on quantity of services rather than high-quality care, and an emphasis on acute care rather than long-term investments in population and community health.
Kaiser Permanente achieves better outcomes through a combination of care coordination, comprehensive data collection and use, and aligned incentives that all promote affordable, high-quality care. This case study, part of our Integrated Care Stories series, highlights the benefits of Kaiser Permanente’s approach.
Caring for Women at High Risk of Breast Cancer
Learn about Kaiser Permanente’s end-to-end care — from early detection of breast cancer to treatment to survivorship.
Cancer care at Kaiser Permanente
At Kaiser Permanente, you have an experienced team of oncologists, or cancer specialists, working together for all that is you. Our members are 20% less likely to die prematurely of cancer compared with nonmembers in their community.
1 American Cancer Society, Breast Cancer Facts and Figures 2019-2020. Atlanta: American Cancer Society, Inc. 2019.
2 National Cancer Institute, BRCA Gene Mutations: Cancer Risk and Genetic Testing, https://www.cancer.gov/about-cancer/causes-prevention/genetics/brca-fact-sheet, accessed February 1, 2021.
3 Stanford Medicine Cancer Institute, Decision Tool for Women with BRCA Mutations, https://brcatool.stanford.edu/brca.html, accessed February 1, 2021.
4 Andreas Koldehoff, MD, et al., “Cost-Effectiveness of Targeted Genetic Testing for Breast and Ovarian Cancer: A Systematic Review,” Value in Health, February 2021, p. 303, and Elvira D’Andrea, MD, et al., “Which BRCA Genetic Testing Programs Are Ready for Implementation in Health Care? A Systematic Review of Economic Evaluations,” Genetics in Medicine, April 2016, p. 1171.