
Integrated Care Stories
Early warning system for hospitalized patients
Kaiser Permanente achieves better outcomes through a combination of care coordination, comprehensive data collection and use, and aligned incentives that all promote affordable, high-quality care. This case study, part of our Integrated Care Stories series, highlights the benefits of Kaiser Permanente’s approach.
The challenge
In any health system, hospitalized patients sometimes have their condition suddenly and unexpectedly worsen, requiring transfer to the intensive care unit or cardiopulmonary resuscitation outside the ICU. These incidents are associated with higher rates of severe illness and death. To reduce the risk of deterioration, care teams must recognize, communicate, and act quickly to address changes in a patient’s physical and mental health.
The integrated care and coverage solution
The Kaiser Permanente Division of Research led development of a clinical early warning system that addresses this challenge, the Advance Alert Monitor (AAM). Typically, “Code Blues” alert care teams to immediate emergencies, but the AAM’s early warning system gives clinicians 12 hours of extra lead time, allowing a more tailored and effective response.
To develop the system, our researchers used data from over 1.5 million Kaiser Permanente patients to identify scores that indicate the severity of a patient’s illness. The scores are combined with data from the patient’s electronic health record to quantify their risk of rapid deterioration.
If a patient’s risk exceeds a determined threshold, the AAM issues an alert to an off-site, virtual team of specialized, highly trained registered nurses. After an in-depth review of the patient’s condition, the Virtual Quality Team nurse contacts the Rapid Response Team nurse at the patient’s bedside. The Rapid Response Team nurse then works with the physician, nurse, social worker, and/or palliative care professional to adjust the patient’s care plan to reduce the risk of deterioration and to ensure that the patient’s preferences are respected.
The AAM program has been implemented in all 21 Kaiser Permanente hospitals in Northern California. This has facilitated early rescue of patients, reduced ICU length of stay, reduced all-cause mortality, and reduced costs.1
How Kaiser Permanente’s integrated care and coverage model supported this innovation
Flexibility within a budget
The Kaiser Foundation Health Plan collects member premiums in advance and then pays delivery system partners for members’ care throughout the year. This creates the flexibility within and across the health plan, the hospitals, and the medical groups to deploy those resources to best meet our members’ needs. Instead of relying on revenues generated when patients are sick, we are incentivized to invest in longer-term infrastructure and population health investments that improve long-term outcomes, and to provide timely, effective, and efficient care and service.
Leadership recognized the potential to improve care and reduce costs, and supported physician led efforts to address the problem.
Extensive population-level data
With access to data across large numbers of patients over long periods of time, Kaiser Permanente tracks population health trends, and identifies and pursues opportunities to improve and to eliminate disparities in care.
Kaiser Permanente analyzed data from over 1.5 million of our patients to develop the scores AAM uses to identify and address high risks of patient deterioration in the hospital.
Research and quality improvement
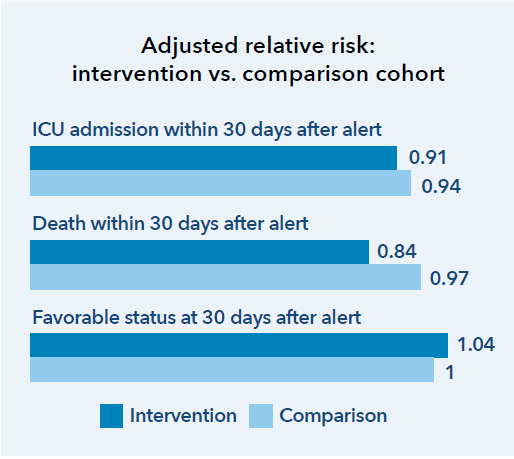
The recent study published in the New England of Journal Medicine found that the system was responsible for preventing 520 deaths per year over a 3-and-a-half-year study period. It also showed a lower incidence of ICU admissions and shorter hospital stays. We analyze care management processes and outcomes and use these results to continuously improve. We then share findings from this practice-based clinical research to benefit others beyond Kaiser Permanente.
Results and reflections on growing the program were also highlighted in the Joint Commission Journal on Quality and Patient Safety, and recently earned the Austco Excellence Award for Quality and Patient Safety at the 2021 International Hospital Federation Awards.
Connected, coordinated care teams
Clinicians can easily coordinate with one another and seamlessly refer patients to other team members — primary care doctors, specialists, lab technicians, pharmacists, and other health care professionals.
Highly trained Virtual Quality Team nurses use AAM data to identify when they need to alert the nurse working directly with the patient. That nurse then coordinates with other care team members to address the identified risk.
Focus on individual and population health
Kaiser Permanente’s mission is to provide high-quality, affordable health care services and to improve the health of our members and the communities we serve. This mission, and our long-term perspective motivates us to address individual and community drivers of health. Investments in individual and population health help us retain our members, and we benefit when those long-tenured members and the broader communities we serve realize positive health outcomes.
The AAM program has improved patient outcomes, including reductions in all-cause mortality rates.
Kaiser Permanente’s integrated care and coverage model differs from much of the United States health care system, which relies on disconnected clinical practices paid through fee-for-service. These disconnected approaches typically result in highly fragmented care, a focus on quantity of services rather than high-quality care, and an emphasis on acute care rather than long-term investments in population and community health.
Kaiser Permanente achieves better outcomes through a combination of care coordination, comprehensive data collection and use, and aligned incentives that all promote affordable, high-quality care. This case study, part of our Integrated Care Stories series, highlights the benefits of Kaiser Permanente’s approach.
How the Advance Alert Monitor works
This video explains how Advance Alert Monitor works for patients.
Behind-the-scenes alert system ‘another set of eyes’
As a neonatal intensive care nurse for 39 years, Erin Fowler-Jones knows what exceptional care looks like. When she arrived at a Kaiser Permanente emergency department in Northern California because of a worsening foot infection, she was impressed by the attention and care she received.
Automated identification of adults at risk for in-hospital clinical deterioration
A New England Journal of Medicine study examines this program.
- Gabriel J. Escobar, MD, et al., “Automated Identification of Adults at Risk for In-Hospital Clinical Deterioration,” The New England Journal of Medicine, November 2020, p. 1951.
- Gabriel J. Escobar, MD, et al., “Automated Identification of Adults at Risk for In-Hospital Clinical Deterioration,” The New England Journal of Medicine, November 2020, p. 1951; and Paulson, RN, et al., “What Do We Do After the Pilot Is Done? Implementation of a Hospital Early Warning System at Scale,” The Joint Commission Journal on Quality and Patient Safety, April 2020, p. 207.